How to loose weight with glucose tracking or the Zoe Program
Track your glucose to learn how to loose weight.
We think everyone should track their glucose, because if you understand how to interpret the glucose data properly, it allows you to use it to loose weight, reduce appetite and food cravings, and banish fatigue.
If you’re feeling like you can’t lose weight, despite eating healthily and exercising, this will be the right method for you. You may even have tried fasting or restricting, but it’s not having much effect. Your metabolism feels slow, and the weight is not shifting no matter what.
Despite doing everything you’ve read you should do, you feel more heavy, bloated, puffy and sluggish. Glucose tracking is free - so what are you waiting for?
Glucose Monitoring for Weight Loss
If you have been a yo-yo dieter, that first ever diet you went on probably disrupted your appetite and connection with food somewhat.
You’ve then entered the modern world of convenience food, which disrupts your metabolism (how we burn fat). Stress, snacking and eating too many ‘fast carbs’ drive up our glucose and insulin - the mechanism underlying this metabolic dysfunction.
Glucose monitors are designed for diabetics, but have been used in our clinic one one form or another for over a decade. With the access to free continual glucose monitors - which you simply pop on your arm without any blood being drawn, we’ve significantly upgraded the type of health -data we can access, and the simplicity of which to gather this. You stick it on, eat as normal - making some notes as you go. The data then gets sent over to one of our practitioners who can then tell you if your diet is causing you to more hungry, brain fogged and tired. The value of tracking blood glucose extends well beyond diabetes management, offering valuable insights into various facets of well-being, including how your diet is negatively impeding your metabolic rate, to how you sleep and how your lifestyle is impacting your ability to stay lean.
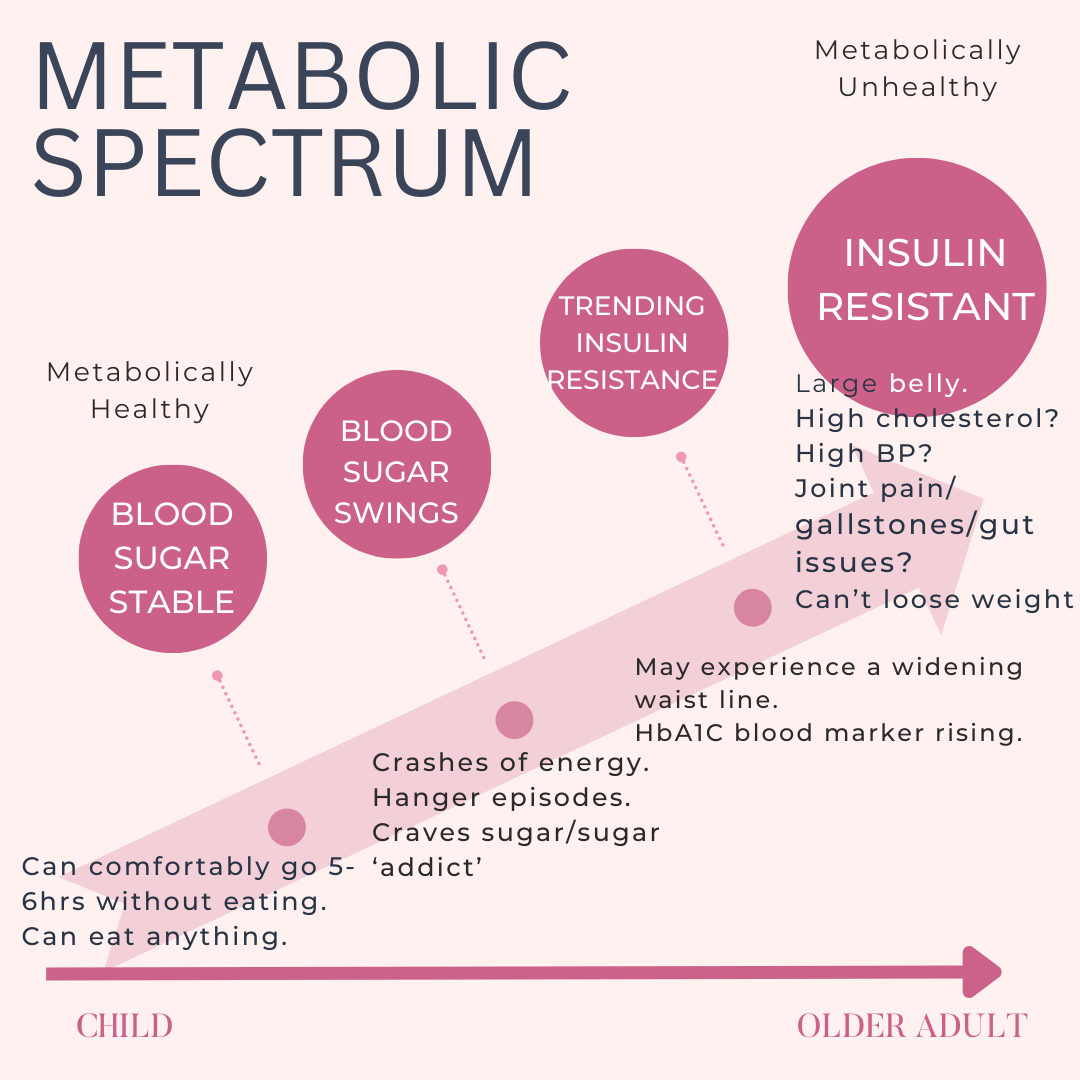
Your Metabolic Spectrum & Insulin Resistance
Metabolic health is a spectrum and a trajectory. We start off as healthy, metabolically flexible toddlers who eat as and when. As we age, we increasingly get set in our routines, with more regular eating and with food rewards harder to resist, we can become increasingly insulin resistant, raising what' we’ve coined your ‘Metabolic Spectrum’ score. Why do we care? Well because not only does a poor metabolic spectrum score mean you can be more insulin resistant**, it also typically means weight gain and ‘food addiction’ (in the sense of not being able to stop eating or eating certain foods).
By the time we are of old age, many of us will be mildly diabetic or pre-diabetic. Understanding one's place on this spectrum is pivotal for effective health preservation and the prevention of chronic conditions, and glucose monitoring can help us do that. Are you metabolically healthy, or mildly insulin resistant - or even at pre-diabetic stage? We want to be at the metabolically flexible toddler stage throughout - this is the nirvana. You eat when you want, and what you want, because appetite and portions are naturally balanced. Hunger will simply feel like a vague gnawing feeling in the tummy, and you will feel less need to eat.
What is insulin resistance?
Over time, if we over-eat simple/fast/processed carbohydrates, the body’s metabolic rate - i.e how it regulates energy storing versus using up energy - begins to struggle. Insulin no longer works effectively, and the body pumps up more as a response- preventing fat loss and increasing weight, often around the middle and waist. We call this metabolic syndrom or metabolic dysfunction. In this scenario, cells become less responsive to insulin due to the constant production (snacking?). If you’re diabetic, the situation is more severe, and the pancreas struggles to keep up it’s normal function and ability to produce insulin. This creates persistently high blood sugar - and damage to the body. Insulin resistance is also very inflammatory, and can increase joint pain and all other types of pain. We know that this scenario is a driver in obesity, which of course affects millions (650million as of current date) of people around the world. The risk of chronic diseases of all kinds are increased in obesity, from cancer, heart disease as well all know, but also fatty liver disease and PCOS in women. Given that some of these disases are largely preventable therefore, justifices taking steps to prevent. Prevention is definitely easier than ‘cure’ as they say, and this is very much true in these cases. Not to mention how much more you’ll be able to live a fulfilling and joyful life, more free with the stress and anguish that comes with fighting a battle of weight and weight loss.
The CGM delivers extremely insightful data for the client. It also alllows your practitioner to be really precise about what you need to change in the diet, to get your metabolism to a better place. It uncovers ‘secrets’ into how your body is reacting to very specific foods, meal timings and habits. Your body may have unique responses to your lifestyle.
Can’t you measure your glucose at your GP?
Regretfully, healthcare is typically mostly ‘reactive’ as oppose to proactive, only kicking in once borderline diabetes has already developed. If you want to have better health and have an easier time managing your weight - this is far too late. It’s also is a much harder turnaround for people once they’re pre-diabetic, when cravings, appetite and emotional attachment tend to be increased. In this scenario, you’re ‘fullness feeling’ signals to your brain has changed, making stopping eating much harder for an obese person than a slim person. Ad on top of that many years of restricting and dieting, which actually tends to reinforce feelings of emotional attachment to ‘reward-foods’ and increase the challenge.
Routine check-ups involve standard blood tests, but you may not be informed that you’re trending towards insulin resistance (poor metabolic rate), nor would your GP necessarily have the resources to support you to make the dietary changes that you need to do.. We urge you to ask to see your blood results, and do your own research, taking charge of your health outcome. Sadly, the public health messages around processed carbohydrates and diabetes or metabolic rate were not adequate (some might say incorrect, as it up until relatively recently recommended a low fat and high carbohydrate diet!) for decades, and political forces are highly motivated by corporate and commercial food industry interests. Whilst the research is all there and there’s no debate, this hasn’t trickled down to the public in any way, in fact it’s barely made it to healthcare givers at large.
How can you tell if your metabolism has started to decline?
The decline in metabolic health often occurs without obvious symptoms, in particular at early stages (often in your 20s). Your cholesterol may start to creep up if you’re in your 40s, and your waist line may not be what it use to be. If you’re in your 20s, you may simply notice cravings, ocassional night waking, PMS and blood sugar drops. We know that the population at large would benefit from understanding their health risk and these vital health markers, and we would argue that most adults would benefit from this deep health screen.
What about our BMI - is this a good indicator of our metabolic rate?
Contrary to popular belief, a high Body Mass Index (BMI) is not always a good indicator metabolic health. A more useful tool in fact, would be the ‘Waist-to-hip ratio’. This can be a good indicator on whether your insulin resistance and metabolic score is worsening. This can be particularly useful in an otherwise slim person, where a widening waistline may be the only sign. It’s also considered to be a marker of cardiovascular disease risk, so it’s something you should be paying attention to.
How Can We Manage Something We Don’t Measure?
Monitoring blood glucose offers both immediate and long-term data directly tied to our health. There are different ways to monitor, each providing good, but different insights. Some of the methods include the HbA1C blood test (common GP test), Glucose Tolerance Test (only used when pregnant) and the Continuous Glucose Monitor (CGM). Although HbA1C is useful, it lacks the detail of your are reacting in real-time. The use of a CGM stands out by giving glucose data that relates directly to what you’re eating and how you’re living your life - thereby telling us the ‘why’ and the specifics about you as an individual. It’s usefulness in providing insights into how the state of our metabolic rate, and where we are on the metabolic trajectory and spectrum makes it relevant to each and everyone of us, from our 20s and into our old age.
Conclusion
Our metabolic health is intricately tied to our level of wellbeing, and health issues such as fatigue, more severe menopause symptoms and food cravings, and and through vigilant monitoring and thoughtful lifestyle adjustments, individuals can proactively reduce the risk of a huge range of common health conditions. On the journey to optimal health, one can leverage biological data as a guiding tool in ensuring we ultimately have a chance at living a full and healthy life.
If you’re interested in understanding whether you are insulin resistance or have ‘sluggish’ metabolism, we can help! Have questions? Head to our Frequently Asked Questions.
** Note we are not medically trained or a replacement for your GP! Nutriitonists do not diagnose, only a Doctor can do this. If you have any concerns whatsoever about your health or blood sugar, you must see your GP. We work in the realm of health optimisation only.